An impulse control disorder is a condition in which a person has trouble controlling emotions or behaviors. Often, the behaviors violate the rights of others or conflict with societal norms and the law.1
Examples of impulse control disorders include oppositional defiant disorder, conduct disorder, intermittent explosive disorder, kleptomania, and pyromania.2
According to data from the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), about 10.5% of the general population is estimated to have an impulse control disorder.3
Males may be slightly more prone to impulse control disorders than females, and these disorders may commonly co-occur with other mental health disorders or with substance abuse.1
Impulse control disorders may be overlooked or misdiagnosed, meaning that many individuals suffering from these disorders may not get the help they need. A better understanding of the disorder can help close the treatment gap and get individuals proper care to improve symptoms. Treatment for impulse control disorders often involves behavioral therapies, and medications may also be beneficial.
Understanding Impulse Control Disorders

- Intermittent explosive disorder: This disorder, also known as IED, is characterized by persistent impulsive and angry outbursts. The person may be violent or aggressive toward people, animals, or property. These tirades may only last about a half hour and are usually triggered by a minor issue with someone the person knows. The outbursts may result in legal or financial issues, disrupt a person’s interpersonal relationships, cause significant distress, and potentially result in problems at work or school. According to Harvard Health, around 5% to 7% of Americans will suffer from IED at some point in their lifetime.1,2,4
- Oppositional defiant disorder: A person with oppositional defiant disorder (ODD) frequently loses their temper, is easily annoyed, and often becomes angry or resentful. They challenge authority figures, flout rules, bother other people on purpose, and blame other people for their problems. As a result of these behaviors, the person suffers problems at work and school, and socially. Symptoms may appear as early as preschool. The prevalence rate is estimated to be around 3.3%.1,2
- Conduct disorder: Conduct disorder consists of persistent behavior that violates social rules. The person may be aggressive toward people or animals, destroy other people’s property, lie or steal, or violate rules, such as run away or skip school at an early age. The behavior causes serious problems at school or socially. People are usually not diagnosed with this disorder over the age of 18. Adults with these symptoms are diagnosed with antisocial personality disorder. The prevalence rate is estimated to be about 4%.1,2
- Kleptomania:Impulsive and unnecessary stealing of things that are not needed characterizes kleptomania. Individuals may steal things and give them to other people or even throw them away. The disorder is not about the things stolen, but instead about the compulsion to steal and lack of self-control over this compulsion. Individuals may feel a sense of relief or gratification after committing the theft. Legal, family, career, and personal troubles are common for individuals with kleptomania. Between 4% to 24% percent of people who shoplift may suffer from kleptomania, and prevalence in the general population is about 0.3% to 0.6%.1
- Pyromania:An individual who repeatedly and deliberately sets fires may suffer from pyromania. An attraction or obsession with fire and fire-setting paraphernalia, along with a compulsive need to set fires, and relief and pleasure after doing so characterize this disorder. Individuals do not set fires for any other reason other than their compulsion to do so to dispel their mounting tension. Pyromania is considered relatively rare, and the lifetime prevalence of people in the United States who intentionally set fires is reported to be around 3.3%.1
Root Causes
There is no single cause for impulse control disorders. Temperamental, physiological, environmental, and genetic factors may play a role in the development of a disorder.1
- Intermittent explosive disorder—history of physical and emotional trauma, relatives with IED, and serotonin abnormalities in the limbic system and orbitofrontal cortex are possible risk factors and causes of IED.1
- Oppositional defiant disorder—problems with emotional regulation; harsh, inconsistent, and neglectful parenting; reduced basal cortisol reactivity; and abnormalities in the prefrontal cortex and amygdala are possible risk factors and causes of ODD.1
- Conduct disorder—difficult temperament as an infant; below average intelligence; abusive and/or inconsistent parenting; exposure to violence; relatives with conduct disorder, depression, alcohol abuse, bipolar disorder, schizophrenia, or ADHD; and structural and functional differences in the ventral prefrontal cortex and amygdala are possible causes and risk factors for conduct disorder.1
- Kleptomania—relatives with obsessive-compulsive disorder and substance use disorders may be a risk factor for kleptomania.1
Co-Occurring Impulse Control Disorders and Substance Abuse
About 19.7 million people in the United States aged 12 and older battled a substance use disorder in 2017, the National Survey on Drug Use and Health (NSDUH) reports, and about 8.5 million Americans age 18 and older suffered from co-occurring substance abuse and mental health disorders in 2017.5
Impulse control disorders and substance use disorders frequently co-occur. Studies have found that:6
- About 35% to 48% of people with intermittent explosive disorders also have substance use disorders.
- About 33% of people with pyromania also have substance use disorders.
- About 22% to 50% of people with kleptomania also have substance use disorders.
The two types of disorder also share similar features. For example, both impulse control and substance use disorders are characterized by compulsion and a lack of control—over a behavior or use of a substance, respectively. People with either disorder also experience a craving to use the substance or carry out the behavior, and both disorders are believed to involve the dopaminergic “reward system” of the brain.7
Depression and anxiety disorders are also comorbid conditions with impulse control disorders. The National Institutes of Health reports that as many as 82% of people suffering from intermittent explosive disorder have a co-occurring substance abuse, anxiety, or depressive disorder as well.8
How to Get Help for Co-occurring Disorders

The National Survey on Drug Use and Health reports that in 2017, about 94% of people age 12 and older who needed substance abuse treatment but did not receive it did not think that they needed treatment. About 7.4% of people age 18 and older with a mental illness did not think that they needed treatment at the time.5 Less than 20% of individuals battling intermittent explosive disorder actually receive specific treatment for their rage episodes, according to survey results published by Harvard Health.4
Often, a loved one or family member may be able to help the person recognize the need for and the potential benefits of a specialized treatment program. An intervention is a structured meeting between the people in someone’s life who may be impacted by the substance abuse and/or untreated impulse control disorder. Family members, loved ones, coworkers, and other important people in an individual’s life may wish to be involved. The main goal of an intervention is to help the person seek out and enter a treatment program.
Since some impulse control disorders are characterized by aggression, violence, and bouts of rage, it is helpful to have the input and guidance of a professional interventionist who is trained to plan and carry out an intervention for the safety of everyone involved.
Typically, the intervention is planned in advance. Loved ones may write down specific instances where the person’s negative behaviors have impacted them and share them during the meeting. The intervention is meant to be nonconfrontational. Participants should stick to “I” statements, talking about how certain situations made them feel and not point fingers.
An interventionist can structure an intervention so it goes smoothly and stays focused on the main goal—getting the person into treatment. The Association of Intervention Specialists (AIS) is a member organization that can help loved ones find a professional interventionist nearby.
Treatment Programs and Methods for Impulse Control Disorders and Substance Abuse
Treatment programs for co-occurring disorders may be either residential, where the person lives on site for a period of time, or outpatient, where the person attends treatment for some portion of the day and goes home at night.
Inpatient or residential programs often consist of individual and group therapy, some level of medical care, supplemental/alternative therapies such as art therapy or meditation, and 12-step meetings. Residents also participate in activities together such as movie nights or outdoor recreation.
Outpatient programs can vary in their structure. Partial hospitalization programs are similar to residential programs in structure and schedule during the day, with the main difference being that the person returns home each night. More flexible outpatient programs can be structured to fit a person’s existing schedule and life obligations.
The intensity and duration of symptoms, potential severity of a person’s dependence on a psychoactive substance, and other factors such as physical health dictate what type of treatment program would be best. For example, some people may require a period of detox before they begin treatment. Detox is sometimes available at inpatient/residential programs but can also be done in standalone facilities or hospitals.
In the case of co-occurring disorders, integrated treatment is considered superior when compared to separate treatment for each disorder.9 This type of treatment takes both disorders into account.
Impulse control disorders and drug or alcohol addiction may be treated with a variety of therapies within a treatment program.9
- Cognitive behavioral therapy (CBT) is a widely used form of therapy that helps individuals to learn how to modify potentially detrimental thought patterns and behaviors.
- Dialectical behavior therapy helps people control self-harm behaviors such as suicidal attempts, thoughts, or urges, as well as drug use.
- Contingency management offers rewards for engaging in healthy behaviors or avoiding unhealthy behaviors such as drug use.
Therapy can take place in an individual, group, or family setting. For parents of adolescents or children with impulse control disorders, treatment may also include working with the parents on how to respond to their child’s behaviors in a positive manner.2
 Medications may aid in the treatment of impulse control disorders, but no drugs are specifically approved to treat these disorders.
Medications may aid in the treatment of impulse control disorders, but no drugs are specifically approved to treat these disorders.Selective serotonin reuptake inhibitors (SSRIs) are antidepressant medications that have been studied for the treatment of impulse control disorders. For example, Frontiers in Psychiatry reported improvement in aggression and irritability in people battling intermittent explosive disorder who took Prozac (fluoxetine).6
The opioid antagonist drug naltrexone, which is often used in the treatment of opioid dependence, may be useful in treating kleptomania as well as addiction. Other medications such as glutamatergic agents and mood stabilizers are also being researched for the treatment of these disorders.6
Medications can also be used for other disorders that people will impulse control disorders and substance abuse may struggle with such as attention-deficit hyperactivity disorder (ADHD), depression, or anxiety.2
Starting Recovery
If you or someone you care about is struggling with an impulse control disorder and/or substance abuse, contact us today at
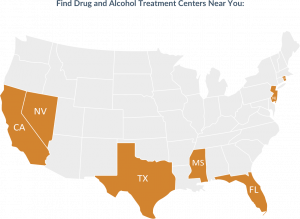
for more information about treatment options at American Addiction Centers.Find Drug and Detox Treatment Centers Near You
Sources
[1]. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
[2]. American Psychiatric Association. (2018). What Are Disruptive, Impulse-Control and Conduct Disorders?
[3]. Harvard Medical School. 12-month prevalence of DSM-IV/WMH-CIDI disorders by sex and cohort.
[4]. Harvard Medical School. (2011). Treating intermittent explosive disorder.
[5]. Substance Abuse and Mental Health Services Administration. (2018). Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health.
[6]. Schreiber, L., Odlaug, B., and Grant, J. (2011). Impulse Control Disorders: Updated Review of Clinical Characteristics and Pharmacological Management. Frontiers in Psychiatry, 2(1).
[7]. Probst, C. and Eimeren, T. (2013). The Functional Anatomy of Impulse Control Disorders. Current Neurology and Neuroscience Reports, 13(10), 386.
[8]. National Institutes of Health. (2006). Intermittent Explosive Disorder Affects Up to 16 Million Americans.
[9]. National Institute on Drug Abuse. (2018). Common Comorbidities with Substance Use Disorders.
